Functional Movement Screen™ and Ankle Stability
Mary A. Dunyak
Meredith College
Abstract
More injuries occur in the ankle than any other bodily joint (Fong, Hong, Chan, Yung & Chan, 2007), and those injuries often lead to symptoms of instability (Yeung, Chan, So, & Yuan, 1994). The Functional Movement Screen™ (FMS™) has advertised itself as a tool to identify an individual's risk of injury. The purpose of this research was to determine if the FMS™ could be a valid tool for predicting ankle injury, by exploring if a relationship exists between the FMS™ and ankle stability. Sixty individuals, aged 18-25, participated in this study. Each participant took part of an FMS™, as well as the Balance Error Scoring System (BESS) test as the measure of ankle stability. Correlations were utilized to analyze the results. Results showed that the FMS™ may not be the best tool as an ankle injury screen. Because the FMS™ is often performed in sport performance or physical therapy settings, this research may provide insight to the usefulness of this screen in those settings.
Introduction
Over one-third of injuries occur in the ankle joint, and ankle sprains are estimated to account for 50 to 76 percent of all ankle injuries (Fong et al., 2007; Garrick & Requa, 1988). Furthermore, up to 73 percent of ankle sprains will result in instability symptoms (Yeung et al., 1994). Because ankle injuries are so prevalent and often lead to chronic symptoms, the ability to identify an individual's ankle injury risk would be useful in preventing injuries.
Functional Movement Screen™ (FMS™)
The purpose of the Functional Movement Screen™ (FMS™) is to predict and therefore prevent any potential injuries (Cook, Burton, Hoogenboom, 2006a). The screen involves the participant performing seven common movements that are functional in everyday actions. Specifically, the screen discerns the body's stability, flexibility, and asymmetries. The result of a FMS™ can show which specific movement deficiency the participant has, which can help therapists and coaches specify what movements need correcting. The FMS™ has strong intra-rater reliability (Gribble, Brigle, Pietrosimone, Pfile, & Webster, 2013; Shultz, Anderson, Matheson, Marcello, & Besier, 2013).
Several studies have shown that a high FMS™ score accurately in predicting a lower injury occurrence (Chorba, Chorba, Bouillon, Overmyer & Landis, 2010; Kiesel, Plisky, & Voight, 2007), which agrees with the FMS™ methodology (Cook et al., 2006a). More recently, O'Connor, Duester, Davis, Pappas, & Knapik (2011) found a disparity in this argument as some higher FMS™ scoring individuals had a higher injury occurrence than those who scored lower.
Research is lacking on the FMS™ and its ability to identify injuries of a specific joint. Instead, the focus of previous research has been on injury risk as a whole.
Present Study
Ankle injuries occur while the body is in motion, which is how the FMS™ evaluates injury risk. The purpose of this study was to determine whether or not the FMS™ is a valid tool in measuring a person's ankle stability. Specifically, the researcher addressed whether a relationship existed between total FMS™ score and ankle stability. The researcher further examined whether this relationship differs based off of the individual's injury history and gender.
Methods
For this study, the researcher administered the FMS™ first, followed by the Balance Error Scoring System (BESS) as a measure of ankle stability.
Subjects
The participants of this study included 60 adults, male and female, between the ages of 18 and 25. Prior to the start, the participants signed an informed consent that was approved by an Institutional Review Board.
Instruments and Test Equipment
A FMS™ kit was used for the screen administration. A 20" x 16.4" x 2.5" Airex foam pad was used for the BESS. For timing each stance, an iPhone stopwatch was used.
Procedures
The testing began once the participant signed the informed consent. The participants were asked to remove their shoes prior to being tested in order to eliminate any extra stability. The experimenter then recorded any of the participant's previous injuries. In order for an injury to be considered, it had to have been doctor-diagnosed and occurred in the hip, knee, or ankle joint.
FMS™. The measurement for the FMS™ was based on the guidelines outlined by Cook and colleagues (2006a). In this study, only four of the movements were performed. Research shows that performing part of the screen is just as predictive of injury as performing the full screen (O'Connor, Deuster, Davis, Pappas, & Knapik, 2011). The movements chosen all utilized the ankle joint: the deep squat, the hurdle step, the in line lunge, and the active straight leg raise.
Each movement of the FMS™ was scored on a scale of 0-3. The participant got three attempts to complete each movement, and the highest scoring attempt counted. A score of three indicated that the movement was performed correctly. A score of two specified that the movement was successfully performed, but done so in a less efficient way. A score of one meant that the participant could not complete the movement. A score of zero was only given when the participant experienced pain throughout the movement. At the conclusion of the FMS™, the four movement scores were summed to obtain the participant's total FMS™ score. For the purpose of this study, the maximum score that an individual could earn was 12.
The experimenter's job while administering the test was to make sure the participant knew what movement to do without being coached into performing it correctly. This was important in ensuring that the participant performed the movement naturally. The experimenter used partial demonstration of the movement rather than complete demonstration. If the researcher was stuck between two scores, the lower score was given. When scoring a bilateral movement, the experimenter scored each side separately and chose the lower of the two sides for the movement's final score.
Deep squat. The first movement was the deep squat. Participants began standing with their feet shoulder-width apart. The subjects held the dowel across the top of their head with their elbows at a ninety-degree angle. On a cue by the experimenter, the participants pressed the dowel up until their elbows were extended, squatted as deeply as possible, and then returned to the start position. The purpose of this movement was to look at the closed kinetic chain movement of ankle dorsiflexion, knee flexion, hip flexion, thoracic spine extension, and shoulder flexion and abduction. Specifically at the ankle joint, the ankle's range of motion in dorsiflexion was tested.
There are several parts of the movement that the experimenter examined. The dowel had to remain above the participant's feet the entire time, as dowel movement in the sagittal plane reduced the score. The participant's femur had to drop below horizontal. The participant's knees had to stay aligned above the feet. The absence of any of these cues resulted in a lower score.
If participants performed the movement correctly, they received a score of three. If the experimenter found any error with the movement pattern, the next step was to have participants perform the deep squat with their heels raised along the side of the board with their forefeet on the ground. If the participants performed the movement correctly with their heels raised, then they were awarded a score of two. If the movement still had errors to it, then they were awarded a one. If the participants felt pain at any point during the test, then they were awarded a zero.
Hurdle step. The hurdle step is the first of the bilateral movements. The experimenter first measured the height of the participant's tibial tuberosity from the ground, using the ruler on the dowel. The experimenter then set up the equipment so that the hurdle was aligned with the height of the tibial tuberosity. The subjects started standing with their toes against the back of the board. The dowel was placed across the shoulders behind the neck, with the subjects lightly holding it. The participants then stepped over the hurdle, lightly tapped their heel on the ground in front, and then returned to the starting position. The leg that was stepping over the hurdle was considered the "scoring side." The participants performed the movement three times on each leg. The hurdle step observed single-leg stability, as well as stability in the knees and hips.
The experimenter was observing alignment of the lower extremities during the stepping motion. Therefore, it was important to look for the hip, knee, and ankle to move exclusively within the sagittal plane. It was also important that the participants limited spinal movement and kept the dowel parallel to the floor for the entire movement.
If the moving leg stayed aligned in the sagittal plane, with the participants showing no torso movement, then they received a score of three. If either of these errors were noted, then the participants received a score of two. If the participants could not complete the movement, they received a score of one. A score of zero was only awarded if the subjects experienced pain at any point during the movement.
In-line lunge. The in-line lunge tested the participant's torso and knee stability, quadriceps flexibility, and hip and ankle stability and mobility. The participants began standing on the board with one foot in front of the other. The distance between the feet matched the height of the hurdle used in the hurdle step movement. The dowel was set along the participant's spine, with one hand holding at the cervical spine, and the other holding at the lumbar spine. The arm on the cervical spine corresponded with the leg that was in the back. The instructor asked the participants to lunge, tap their back knee on the board, and then return to the starting position. It was important that the dowel remained in three points of contact throughout the movement (at the cranium, thoracic spine, and sacrum).
The in-line lunge measured many movement pattern deficiencies. It observed the hip, knee, and ankle stability, as well as calf and quadriceps flexibility. It also required core stability. Throughout the movement, the dowel must have kept three points of contact. The torso also had to remain straight and free from any transverse movement. The participants must have been able to touch their knee to the board keeping their feet flat. The feet and knees had to avoid any internal or external rotations, keeping movement in the sagittal plane.
If the participants performed the movement correctly, then they were awarded a score of three. If any of the above movement deficiencies occurred, then they were awarded a two. If the participants could not complete the movement, they were awarded a score of one. Examples of a person unable to complete the movement were extreme loss of balance, not being able to get into the start position, or not being able to return to the end position. A score of zero was awarded if the participants experienced pain at any moment during the test.
Active straight leg raise. The active straight leg raise (ASLR) test observed the flexibility and ability to isolate the hamstring gastroc-soleus complex. The participant began lying supine in anatomical position with the board positioned underneath the participant's knees. The experimenter found the midpoint between the anterior superior iliac spine (ASIS) and the mid-patella, and held the dowel upwards next to that spot. On the experimenter's cue, the participants extended both knees, dorsiflexed both ankles, and maximally lifted one leg. It was important that no external rotation occurred on the non-scoring side.
The participants were scored based on the position of their malleolus when their leg was raised maximally. If the participants' malleolus was located between the dowel and their ASIS, then they were scored a three. If the participants' malleolus was between the dowel and their mid-patella, then they were scored a two. If their malleolus could not reach the mid-patella line, then they were scored a one. If they experienced pain at any point during the test, then they will be scored a zero. It was important to note that the participants were scored at the position that the malleolus reached before external rotation of the opposite hip.
Balance Error Scoring System (BESS).
The Balance Error Scoring System (BESS) has recently shown to be a valid measure of ankle stability (Bell, Guskiewicz, Clark & Padua, 2011). Docherty, Valovich McLeod, & Shultz (2006) were the first to demonstrate that the BESS could identify ankle instability in an individual. The protocol that the researcher used for the BESS was outlined by Bell and colleagues. The BESS test used three stances on two different surfaces to measure ankle stability. The researcher utilized a script during the BESS portion of the study to ensure that all participants were given the same cues.
All stances required the participants to place their hands on their hips and close their eyes for the duration of the stance. The first stance was the double leg stance, which required the participants standing with their feet together. The second stance was a single leg stance, where the participants balanced on their non-dominant leg. The participants held their dominant leg off the ground at thirty degrees of hip flexion and forty five degrees of knee flexion. The third stance was the tandem stance, where the participants balanced with their dominant leg in front of their non-dominant, standing heel to toe. All three stances were performed in that order on a hard floor first. The participants then repeated all three stances on the Airex pad. The participants had to remain in their position for twenty seconds. Timing started with the participants' eyes closing.
During each twenty-second period, the researcher counted the number of errors that the individual made. An error was defined as
- Opening the eyes.
- Lifting the hands off of the hips.
- Stepping, or stumbling out of position.
- Lifting forefoot or heel.
- Abducting the hip more than thirty degrees.
- Failing to return to the test position in more than 5 seconds (Bell et al., 2011).
The researcher recorded the number of errors for each individual stance. The researcher then summed the six scores together to create the total BESS score. The BESS has been shown to have good intra-rater reliability (Finnoff, Peterson, Holloman & Smith, 2009).
Design and Analysis
The purpose this study was to determine if the FMS™ was a valid tool for measuring ankle stability. High FMS™ scores are associated with a lower risk for injury. Low BESS scores are associated with good ankle stability. The experimenter's goal was to compare the FMS™ and BESS scores to see if any relationships exist through the use of correlations.
Results
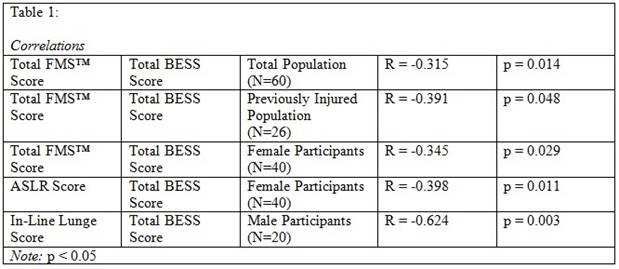
The researcher ran a series of correlations, which can be found in Table 1. Results show a series of negative moderate correlations when significant relationships were found. These correlations were seen across the whole population, previously injured participants, and female participants. The moderate correlation suggests that the relationship between the two variables is not entirely strong. Therefore, this suggests that the FMS™ may not be a valid way to determine a person's likelihood of ankle injury. No significant data were found for male participants, so no conclusion can be made for this population.
The researcher further investigated if any of the individual FMS™ movements showed a relationship with ankle stability in any of the populations. Only two significant relationships were found. A negative moderate correlation was observed among female participants performing the ASLR movement, suggesting that this movement may not be able to identify ankle stability. A negative large correlation was observed between male participants and the in-line lunge movement. This suggests that the in-line lunge movement may be useful in identifying ankle instability symptoms in the male population.
Discussion
Limitations
Several potential limitations existed within this study, which include the environment, the definition of "injury," and the population. Due to the nature of this study, not all of the tests were performed in the same environment. Although the researcher attempted to duplicate the environment as much as possible, the results could have been affected by inconsistencies in testing environment, including the spacing, lighting, temperature, and flooring surface. Another limitation was the broad definition of an injury. A wide variety of injuries were included in this study. The severity of the injury could have easily affected how the participants performed during this test. Furthermore, some participants could have received therapy for their injuries, which research has shown improves symptoms of ankle instability (Hale, Hertel & Olmsted-Kramer, 2007). However, the researcher did not collect this information from participants and therefore, cannot assume that therapy could have affected this research. A final limitation of this study could have been the activity level of the participants, which ranged from completely sedentary individuals to division one NCAA athletes. Some participants indicated that they had performed an FMS™ test prior to participating in this study, which research has shown can increase performance during future testing (Frost, Beach, Callaghan, & McGill, in press).
Future Research
Further research on this subject should limit the injuries to ankle sprains. Due to lack of time and participants, the researcher was unable to isolate ankle sprains in their own injury category. However, when investigating the prevalence of ankle instability, ankle sprains should be the main injury investigated because they are the common result of having an unstable ankle.
Practical Applications
The FMS™ is commonly used in several clinical settings as a tool for assessing movement quality and risk of injury. Despite its purpose, this study found that the FMS could not distinguish which individuals had lower ankle stability. With the high occurrence of ankle injuries, it is important for clinicians to know that the FMS™ may not be an effective way of identifying the risk factors for injuries of this joint. However, while evaluating any joint for injury, the researcher supports the claim that functional evaluation is important in determining how the joint functions in real-life movement situations. Clinicians should investigate other means of functionally evaluating the ankle joint in working with their patients.
References
Balance Error Scoring System (BESS). Retrieved from: http://www.sportsconcussion.com/pdf/management/BESSProtocolNATA09.pdf
Bell, D. R., Guskiewicz, K. M., Clark, M. A., & Padua, D. A. (2011). Systematic Review of the Balance Error Scoring System. Sports Health, 3(3), 287-295.
Chorba, R. S., Chorba, D. J., Bouillon, L. E., Overmyer, C. A., & Landis, J. A. (2010). Use of a Functional Movement Screening Tool to Determine Injury Risk in Female Collegiate Athletes. North American Journal of Sports Physical Therapy, 5(2), 47-54.
Cook, G, Burton, L, & Hoogenboom, B. (2006a). Pre-Participation Screening: The Use of Fundamental Movements as an Assessment of Function- Part 1. North American Journal of Sports Physical Therapy, 1(2), 62-72.
Docherty, C. L., Valovich McLeod, T. C., & Shultz, S. J. (2006). Postural control deficits in participants with functional ankle instability as measured by the balance error scoring system. Clinical Journal of Sport Medicine, 16(3), 203-208.
Finnoff, J. T., Peterson, V. J., Holloman, J. H., & Smith, J. (2009). Intrarater and interrater reliability of the Balance Error Scoring System (BESS). P M &R: the Journal of Injury, Function, and Rehabilitation, 1(1), 50-54.
Frost, D. M., Beach, T. A. C., Callaghan, J. P., & McGill, S. M. (in press). FMS™ scores change with performers' knowledge of the grading criteria – Are general whole-body movement screens capturing "dysfunction"?. Journal of Strength and Conditioning,
Fong, D.T., Hong, Y., Chan, L.K., Yung, P.S., & Chan, K.M. (2007). A Systematic Review on Ankle Injury and Ankle Sprain in Sports. Sports Medicine, 37(1), 73-94.
Garrick, J. G. & Requa, R. K. (1988). The Epidemiology of Foot and Ankle Injuries in Sport. Clinics in Sport Medicine.7(1), 29-36.
Gribble, P.A., Brigle, J., Pietrosimone, B. G., Pfile, K. R., & Webster, K. A. (2013). Intrarater reliability of the functional movement screen. Journal of Strength and Conditioning Research, 27(4), 978-981.
Hale, S. A., Hertel, J., & Olmsted-Kramer, L. C. (2007). The Effect of a 4-Week Comprehensive Rehabilitation Program on Postural Control and Lower Extremity Function in Individuals with Chronic Ankle Instability. Journal of Orthopaedic & Sports Physical Therapy, 37(6), 303-311.
Kiesel, K., Plisky, P., & Voight, M. (2007). Can Serious Injury in Professional Football be Predicted by a Preseason Functional Movement Screen?. North American Journal of Sports Physical Therapy, 2(3), 147-158.
O'Connor, F. G., Deuster, P.A., Davis, J., Pappas, C.G., & Knapik, J. J. (2011). Functional Movement Screening: Predicting Injuries in Officer Candidates. Medicine & Science in Sports & Exercise, 43(12), 2224-2230.
Shultz, R., Anderson, S. C., Matheson, G. O., Marcello, B., & Besier, T. (2013). Test-retest and interrater reliability of the Functional Movement Screen. Journal of Athletic Training, 48(3), 331-336.
Yeung, M. S., Chan, K., So, C. H., & Yuan, W. Y. (1994). An epidemiological survey on ankle sprain. British Journal of Sports Medicine, 28(2), 112-116.
|